Chapter 12 Download Chapter
Performing the Sterilization Procedure
Explaining the Procedure
A woman who has chosen female sterilization needs to know what will happen during the procedure.The following description can help to explain the procedure to her. Learning to perform female sterilization takes training and practice under direct supervision.Therefore, this description is a summary and not detailed instructions.
(The description below is for procedures done more than 6 weeks after childbirth. The procedure used up to 7 days after childbirth is slightly different.)
The Minilaparotomy Procedure
- The provider uses proper infection-prevention procedures at all times (see Infection Prevention in the Clinic, in Chapter 26 – Family Planning Provision).
- The provider performs a physical examination and a pelvic examination. The pelvic examination is to assess the condition and mobility of the uterus.
- The provider inserts a special instrument (uterine elevator) into the vagina, through the cervix, and into the uterus to raise each of the 2 fallopian tubes so they are closer to the incision.This may cause discomfort.
- The woman usually receives light sedation and analgesia to relax her. She stays awake. Local anesthetic is injected above the pubic hair line. She will not experience serious pain.
- The provider makes a small horizontal incision (2–5 cm) in the anesthetized area. This usually causes little pain. (For women who have just given birth, the incision is made at the lower edge of the navel.)
 Each tube is tied and cut or else closed with a clip or ring.
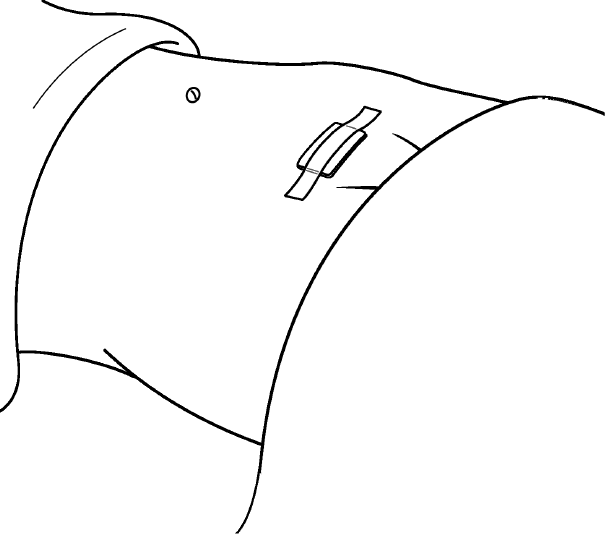
Each tube is tied and cut or else closed with a clip or ring.- The provider closes the incision with stitches and covers it with an adhesive bandage.
- The woman receives instructions on what to do after she leaves the clinic or hospital (see Explaining Self-Care for Female Sterilization). She usually can leave in a few hours.
The Laparoscopy Procedure
- The provider uses proper infection-prevention procedures at all times (see Infection Prevention in the Clinic, in Chapter 26 – Family Planning Provision).
- The provider performs a physical examination and a pelvic examination. The pelvic examination is to assess condition and mobility of the uterus.
- The woman usually receives light sedation and analgesia to relax her. She stays awake. Local anesthetic is injected under her navel. She will not experience serious pain.
- The provider places a special needle into the woman’s abdomen and, through the needle, inflates (insufflates) the abdomen with gas or air. This raises the wall of the abdomen away from the pelvic organs.
- The provider makes a small incision (about 1 cm) in the anesthetized area and inserts a laparoscope. A laparoscope is a long, thin tube containing lenses. Through the lenses the provider can see inside the body and the 2 fallopian tubes.
- The provider inserts an instrument through the laparoscope (or, sometimes, through a second incision) to close off the fallopian tubes.
- Each tube is closed with a clip or a ring, or by electric current applied to block the tube (electrocoagulation).
- The provider then removes the instrument and laparoscope. The gas or air is let out of the woman’s abdomen. The provider closes the incision with stitches and covers it with an adhesive bandage.
- The woman receives instructions on what to do after she leaves the clinic or hospital (see Explaining Self-Care for Female Sterilization). She usually can leave in a few hours.

Local Anesthesia Is Best for Female Sterilization
|
Local anesthesia, used with or without mild sedation and analgesia, is preferable to general anesthesia. Local anesthesia with sedation and analgesia:
Sterilization under local anesthesia, with or without mild sedation and analgesia, can be done when a member of the surgical team has been trained to provide sedation and analgesia and the surgeon has been trained to provide local anesthesia. The surgical team should be trained to manage emergencies, and the facility should have the basic equipment and medicines to manage any emergencies. Health care providers should explain to a woman ahead of time that being awake during the procedure is safer for her. During the procedure providers should talk with the woman and help to reassure her if needed. The most common anesthetic used is lidocaine (lignocaine). Many different sedatives and analgesics may be used. The dosage of medicines must be adjusted to body weight. Oversedation should be avoided because it can reduce the client’s ability to stay conscious and could slow or stop her breathing. In some cases, general anesthesia may be needed. See Medical Eligibility Criteria for Female Sterilization, for medical conditions needing special arrangements, which may include general anesthesia. |