Infection-prevention procedures are simple, effective, and inexpensive. Germs (infectious organisms) of concern in the clinic include bacteria (such as staphylococcus), viruses (particularly HIV and hepatitis B), fungi, and parasites. In the clinic infectious organisms can be found in blood, body fluids with visible blood, and tissue. (Feces, nasal secretions, saliva, sputum, sweat, tears, urine, and vomit are not considered potentially infectious unless they contain blood.) The organisms can be passed through mucous membranes or broken skin, such as cuts and scratches, and by needle sticks with used needles and other puncture wounds. Infectious organisms can pass from clinics to communities when waste disposal is not proper or staff members do not wash their hands properly before leaving the clinic.
Basic Rules of Infection Prevention
These rules apply the universal precautions for infection prevention to the family planning clinic.
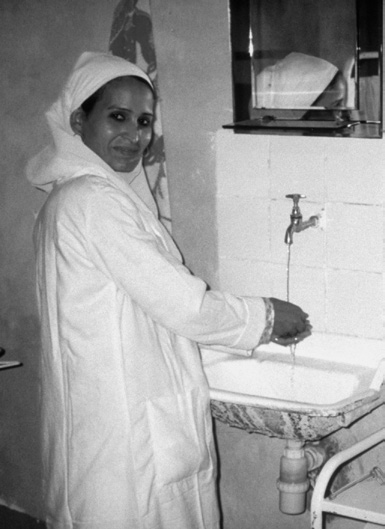
Wash hands
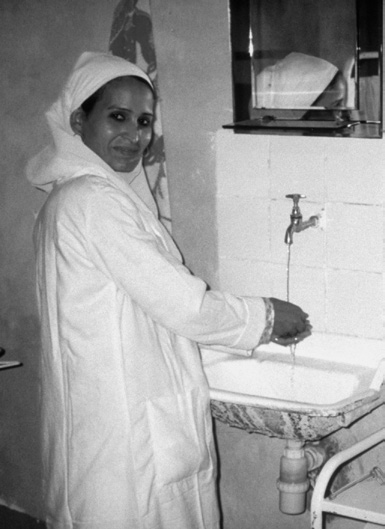 |
- Hand washing may be the single most important infection-prevention procedure.
- Wash hands before and after examining or treating each client. (Hand washing is not necessary if clients do not require an examination or treatment.)
- Use clean water and plain soap, and rub hands for at least 10 to 15 seconds. Be sure to clean between the fingers and under fingernails. Wash hands after handling soiled instruments and other items or touching mucous membranes, blood, or other body fluids. Wash hands before putting on gloves, after taking off gloves, and whenever hands get dirty. Wash hands when you arrive at work, after you use the toilet or latrine, and when you leave work. Dry hands with a paper towel or a clean, dry cloth towel that no one else uses, or air-dry.
- If clean water and soap are not available, a hand sanitizer containing at least 60% alcohol can reduce the number of germs on the hands. Sanitizers do not eliminate all types of germs and might not remove harmful chemicals.
|
| Process instruments that will be reused |
- High-level disinfect or sterilize instruments that touch intact mucous membranes or broken skin.
- Sterilize instruments that touch tissue beneath the skin (see The 4 Steps of Processing Equipment).
|
| Wear gloves |
- Wear gloves for any procedure that risks touching blood, other body fluids, mucous membranes, broken skin, soiled items, dirty surfaces, or waste. Wear surgical gloves for surgical procedures such as insertion of implants. Wear single-use examination gloves for procedures that touch intact mucous membranes or generally to avoid exposure to body fluids. Gloves are not necessary for giving injections.
- Change gloves between procedures on the same client and between clients.
- Do not touch clean equipment or surfaces with dirty gloves or bare hands.
- Wash hands before putting on gloves. Do not wash gloved hands instead of changing gloves. Gloves are not a substitute for hand washing.
- Wear clean utility gloves when cleaning soiled instruments and equipment, handling waste, and cleaning blood or body fluid spills.
|
| Do pelvic examinations only when needed |
- Pelvic examinations are not needed for most family planning methods—only for female sterilization, the IUD, diaphragm, and cervical cap (see Importance of Selected Procedures for Providing Family Planning Methods, in Chapter 25). Pelvic examinations should be done only when there is a reason—such as suspicion of sexually transmitted infections, when the examination could help with diagnosis or treatment.
|
For injections, use new auto-disable syringes
and needles |
- Auto-disable syringes and needles are safer and more reliable than standard single-use disposable syringes and needles, and any disposable syringes and needles are safer than sterilizing reusable syringes and needles. Sterilizing and reusing syringes and needles should be avoided. It might be considered only when single-use injection equipment is not available and the program can document the quality of sterilization.
- Cleaning the client’s skin before the injection is not needed unless the skin is dirty. If it is, wash with soap and water and dry with a clean towel. Wiping with an antiseptic has no added benefit.
|
Wipe surfaces with chlorine
solution |
- Wipe examination tables, bench tops, and other surfaces that come in contact with unbroken skin with 0.5% chlorine solution after each client.
|
Dispose of single-use
equipment and supplies
properly and safely
 |
- Use personal protective equipment—goggles, mask, apron, and closed protective shoes—when handling wastes.
- Needles and syringes meant for single use must not be reused. Do not take apart the needle and syringe. Used needles should not be broken, bent, or recapped. Put used needles and syringes immediately into a puncture-proof container for disposal. (If needles and syringes will not be incinerated, they should be decontaminated by flushing with 0.5% chlorine solution before they are put into the puncture-proof container.) The puncture-proof sharps container should be sealed and either burned, incinerated, or deeply buried when three-fourths full.
- Dressings and other soiled solid waste should be collected in plastic bags and, within 2 days, burned and buried in a deep pit. Liquid wastes should be poured down a utility sink drain or a flushable toilet, or poured into a deep pit and buried.
- Clean waste containers with detergent and rinse with water.
- Remove utility gloves and clean them whenever they are dirty and at least once every day.
- Wash hands before and after disposing of soiled equipment and waste.
|
| Wash linens |
- Wash linens (for example, bedding, caps, gowns, and surgical drapes) by hand or machine and line-dry or machine-dry. When handling soiled linens, wear gloves, hold linens away from your body, and do not shake them.
|
| Low Risk of HIV Infection in the Clinic |
|
Health care providers may be exposed to HIV through needle sticks,mucous membranes, or broken skin, but the risk of infection is low.
- Needle sticks or cuts cause most infections in health care settings.The average risk of HIV infection after a needle-stick exposure to HIV-infected blood is 3 infections per 1,000 needle sticks.
- The risk after exposure of the eye, nose, or mouth to HIV-infected blood is estimated to be about 1 infection per 1,000 exposures.
Following universal precautions is the best way that providers can avoid workplace exposure to HIV and other fluid-borne infections. Post-exposure prophylaxis (PEP) with antiretroviral medicines will help to prevent HIV infection if a needle stick might have exposed a provider to HIV.
|